Trigger Warning. Let’s keep working to remove the stigma.
Here is a very real article written by someone who has experience PTSD and the issues associated with dealing with it. There are many things that need to be done to address this injury and the purpose of this article is to let others know that they are not alone.
Please stay in the fight! Please don’t ever give up even when you’re at your worst, reach out to those that you trust and remember that whilst it may seem sometimes that things will never get better. They will. Look after your mates and look after you.
Every Six Weeks a First Responder Dies to Suicide. The Next Day They’re Old News.
When a police officer suicides - first responders’ suicide at a rate of once every six weeks – there is always a story in the newspaper the next day, talking about all of these issues. They scream at us - the system needs to change, the policies to help people need to have less red tape… the list goes on. But the next day there’s another news story and we all forget. Those in the blue uniform never forget.
They wait until the next one.
Maybe if the ambulance and police car hadn’t screamed past the bakery that day, Paul would still be in the job. Maybe if those sirens hadn’t caused him to crouch in the corner next to the drinks fridge and cover his face, he would still be arresting criminals. And maybe if his chest hadn’t tightened to the pointhe felt like he was having a heart attack he would still be comforting victims of domestic violence.
But maybe it was there all along and no-one asked if he needed help. Maybe he didn’t feel like he could ask for help.
Paul, 36, was a serving police officer for nineteen years. “It was lunchtime the day after my last night shift for the block. I woke up craving a vanilla slice and the bakery was only at the corner of my street. I handed over my card to pay as the first siren went past. My body froze and the woman behind the counter held my card out for me to take back, but I stared at her, unable to process what she wanted from me. I remember backing away from the counter, the woman kept speaking but I didn’t hear her. The only things I could see and hear in that moment were images of dead bodies being pulled from cars, fires raging because a heater caught fire or the bruises on that mother’s face because her husband didn’t like his dinner.
“That’s when I knew I was at breaking point. This was the moment I broke.”
Paul went to see his GP after he was coaxed from the floor by the woman behind the counter. He got an emergency appointment. He sat in front of the doctor and cried - like so many others before him. He knew the journey towards medical retirement lay before him. “I was afraid I’d be followed by investigators to make sure I wasn’t lying. They were going to make me retell everything over and over to a million different doctors. It happened to my mates. I just never thought it would happen to me. I didn’t think I’d be able to cope. I was terrified.”
He never put the blue uniform on again.
After the suicide of NSW police member, Ashley Bryant in 2013 the coroner failed to make recommendations in relation to the insurance companies who pursued Bryant, stating that it was outside the cope of the inquest. Bryant’s widow broke down after the inquest at the failure to acknowledge the ‘elephant in the room.’ The elephant remains today, nestled quietly in the corner of every police station in the state.
Paul is coming up to his fifth independent psychiatrist assessment to qualify for a permanent disablement payout. “It’s burning hoop after burning hoop you have to jump through. And each time it burns you just that little bit more. They don’t understand or maybe they don’t care about the added stress of having to relive the trauma over and over. How can they not see what this does to a person? They’re psychiatrists. Surely one of them has to say at some point… why is this bloke seeing me when he has already gone through four others? I mean… what are they trying to find?”
Because, for so many that’s exactly how it feels – like a fishing expedition. They want to find that one thing from anywhere other than the job to justify why the job isn’t responsible for the poor mental health of one of their own. “Did your father leave you when you were a toddler? Did you almost get hit by a car when you were five? How’s your relationship with your wife? It’s a barrage of questions with the same answers every time. And that’s before they ask about the jobs that traumatised you. That’s way down the list of priorities.
Thomas has been a GP for over thirty years. He has a front row seat to the pain and trauma of first responders. “My father was a soldier and my uncle a detective. Both now live with the horrors they witnessed and in some cases were a part of. I don’t feel right about turning away police officers when they walk into my rooms. They’re broken, lost and frightened. Growing up with my father and hearing his nightmares through the bedroom wall. That sticks with you.
“And now that I see how police are treated after they are affected with mental illness, I understand why my father never went down that path with the army. Nothing will ever change while the system and policies in place remain unchanged. Imagine being told you aren’t sick, while you have a raging headache, bent over the toilet bowl vomiting.
“I had a patient who experienced extreme bruxism (jaw clenching) as a result of his nightmares and flashbacks. The anxiety and trauma caused his jaw to tighten and damaged his teeth substantially. He tried to claim treatment for this through the insurance providers and was told it didn’t qualify as a symptom of his condition.”
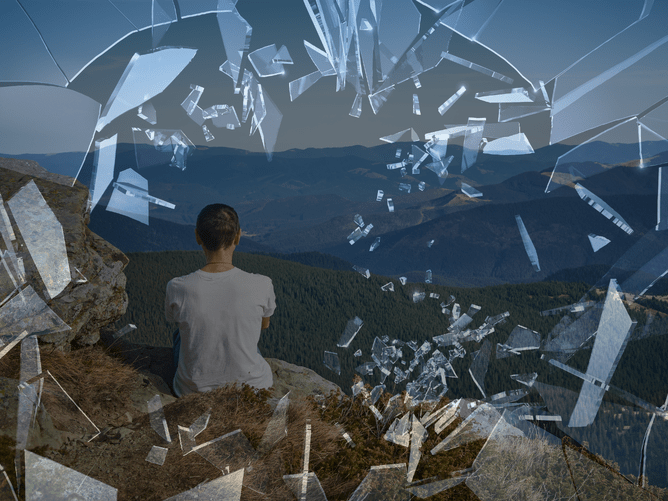
“The loss of identity,” says Thomas. “That’s something that so many police officers struggle with the most. They have been part of this organisation and identified as a police officer for most of their adult life and then all of a sudden they aren’t anymore. That can sometimes be just as confronting as the mental illness. That can be what drives some of them to irreversible choices.”
Current serving officer, Michael, 40, doesn’t know how much longer he has in the job. It’s been two years now that he has told people he needs help and actively pursued it on his own. “There was this one day when I was sitting at my desk, staring at the sticky tape dispenser, and wondering how to dig myself out of the depressed hole I was in. I went to my supervisor and told him in these exact words, I’m really struggling here. I’m not okay. He told me not to worry – I didn’t have to go out on the road today so I could have a “rest”. But then he threw me the keys to the gun safe and asked if I could do the gun check for him, moments after I admitted I was struggling with my mental health.”
Training for mental health and wellbeing care in civilians is ongoing for police officers – for when they’re dealing with mentally ill offenders, victims, or patients they may have to deal with on the street. But where is the training and awareness for their own? It’s online. It’s a few short modules here and there that can be flicked through with the click of a mouse button while speaking to your workmates about that weekend’s footy match.
Michael is reluctant to go off on stress leave or under a workers compensation claim. Why? Because he sees how other colleagues have been treated. He hears the horror stories of insurers psychiatrists telling them they’re just fine and will be able to return to work. And, giving them a low disablement score, which means they get no compensation for their trauma. “I can’t afford to not have this job. But I know the longer I go in every shift and expose myself to more of it, the harder it’s going to be to fix myself. But I don’t have a choice.”
Six years on the other side of medical retirement after a twenty eight year career, stands Patrick, 50. He was discharged at the rank of detective sergeant, and he was part of a number of commands, critical incident investigations and specialist units throughout his career.
“My marriage couldn’t handle my breakdown. I didn’t even realise it was happening. I always loved a drink but apparently it became worse and worse. Margaret couldn’t deal with me after about six months of drinking every single day. She left. I don’t blame her really.”
Patrick considered the police as an extended family. A family that had each other’s back and would be there until the end. What he hadn’t counted on was the lack of contact after he left.
“You are all of a sudden out and alone. Those mates you went through the academy with, had end of shift drinks with, attended horrific jobs with… all of them suddenly go dark on you. I felt like a leper. I’d text or call one of them and get the old let’s catch up soon line. But soon never seems to come.”
Patrick has a mild shake in his hands. It comes from the alcoholism but for him it’s a reminder that he isn’t the same anymore. “I still get nightmares and flashbacks. Not as regularly anymore but when they come they’re intense. It’s like I’m right back there again. I had a thirty year career in the cops. And one of my most vivid flashbacks is from my first week in the job.” The sad smile that takes over his face when he says that seems to set the mood for the rest of the interview. “I’m of that era that doesn’t talk about feeling sad or upset. It just wasn’t the done thing. You pull a dead kid out of a car, and they expect you to not feel it. Or at least not tell anyone how you feel about it. You just have to man up and keep going. But keeping it all bottled up was my ultimate undoing.”
Patrick was involved in some of the highest profile cases we have seen in this state, and each one of them left a mark on him. After too many marks how do you hide those scars? “You drink them away. It’s not ideal but again, it seems to be the culture I was inducted into. Things are different these days, but I still don’t think its enough.”
There are awareness campaigns all the time for mental health. Rugby League commits entire rounds to ask ‘Are you OK?’ and Beyond Blue, Black Dog Institute, Lifeline… all these organisation do what they can to make it okay to talk about your feelings, pain and trauma. After every news story on television about suicide they follow up with the numbers for Lifeline and Beyond Blue. They tell you to go get help.
But for those people who dedicate their lives to helping others and protecting our communities, the help and awareness is lost.
Patrick stares out the window as he sips his tea. “So many young kids in the job are hurting themselves, killing themselves. It shouldn’t happen.”